Inside the Mind of a Psychopath: Exploring Brain Differences
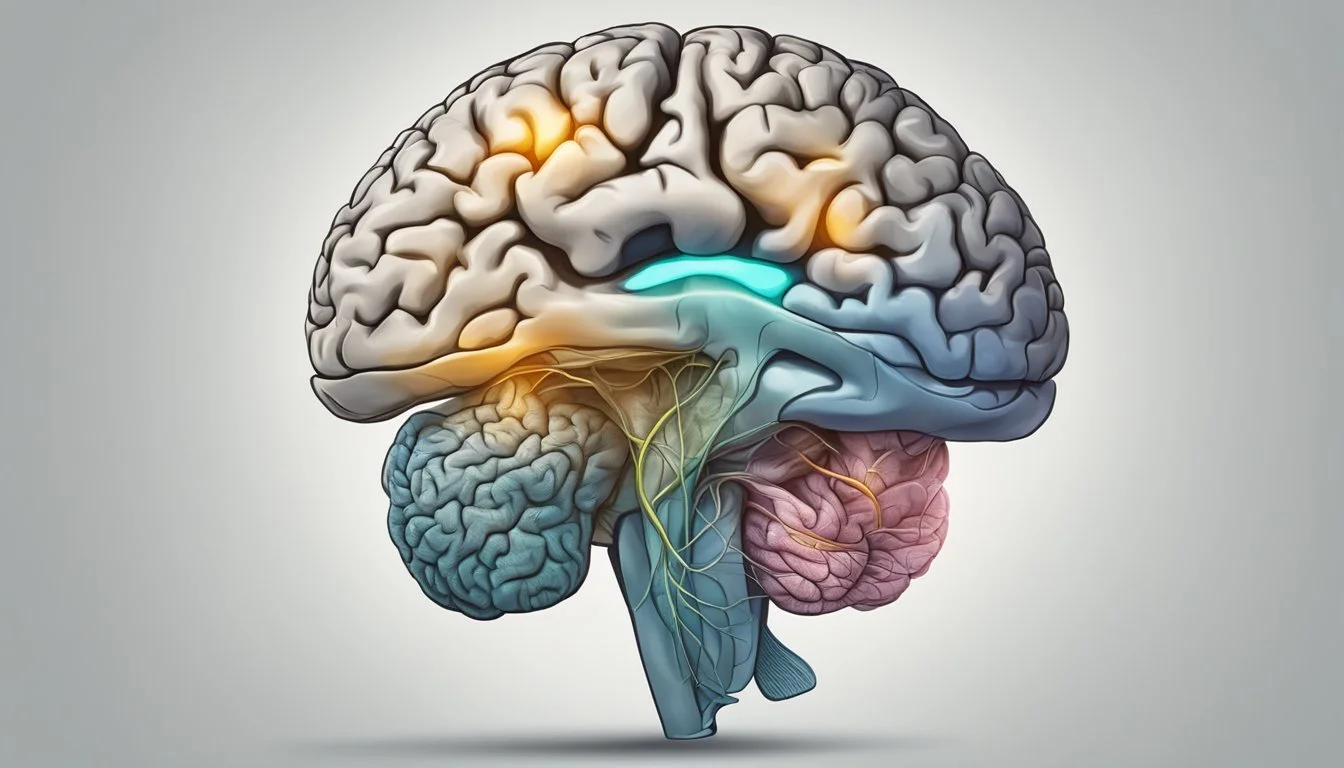
Psychopathy is a complex personality disorder characterized by a lack of empathy, shallow emotions, and antisocial behavior. Recent neuroimaging studies have shed light on the unique brain structure and function of individuals diagnosed with psychopathy. Brain scans reveal reduced connections between the ventromedial prefrontal cortex and amygdala in psychopaths, areas crucial for regulating emotion and social behavior.
These neural differences may contribute to the impaired decision-making and emotional processing observed in psychopathic individuals. While psychopaths make up a small percentage of the population, they are responsible for a disproportionate amount of criminal activity. Understanding the neurobiology of psychopathy could potentially lead to more effective treatments and interventions.
Research into the psychopathic brain has implications beyond the clinical and forensic realms. It provides insights into the neural basis of empathy, morality, and social behavior in the general population. As scientists continue to explore the intricacies of the psychopathic mind, they uncover valuable information about human nature and the complex interplay between brain function and behavior.
Defining Psychopathy
Psychopathy is a complex personality disorder characterized by specific behavioral and emotional traits. It is often associated with criminal behavior but can manifest in various ways across different individuals.
Characteristics of Psychopaths
Psychopaths typically display a lack of empathy and remorse. They often exhibit shallow emotions and are unable to form deep, meaningful relationships.
Charm and manipulation are common traits, used to exploit others for personal gain. Psychopaths may be impulsive and prone to risk-taking behavior.
They frequently demonstrate a grandiose sense of self-worth and are skilled at lying and deceiving others. Psychopaths often fail to accept responsibility for their actions, instead blaming others or external circumstances.
Psychopathic Personality Disorder
Psychopathic personality disorder is not officially recognized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). It shares similarities with Antisocial Personality Disorder but has distinct features.
The disorder is characterized by a persistent pattern of disregard for and violation of others' rights. Individuals with this condition may engage in criminal behavior, display aggression, and lack remorse.
Early signs often emerge in childhood or adolescence. Environmental factors and genetic predisposition may contribute to its development.
Hare Psychopathy Checklist-Revised (PCL-R)
The PCL-R is a widely used diagnostic tool for assessing psychopathy. Developed by Robert Hare, it consists of 20 items scored on a 3-point scale.
The checklist evaluates traits such as glibness, grandiosity, lack of empathy, and criminal versatility. It also assesses behavioral patterns like impulsivity and juvenile delinquency.
Trained professionals administer the PCL-R through interviews and review of collateral information. A score of 30 or above (out of 40) typically indicates psychopathy.
The PCL-R has demonstrated high reliability and validity in forensic settings. It is often used in criminal justice systems to assess risk and inform treatment decisions.
The Psychopath Brain: An Overview
Psychopathy is associated with distinct neurobiological features and alterations in brain structure and function. These differences impact emotional processing, decision-making, and behavior in individuals with psychopathic traits.
Neurobiological Underpinnings
Psychopathy has strong neurobiological roots. Neuroimaging studies reveal reduced gray matter volume in key brain regions. These include the prefrontal cortex, amygdala, and hippocampus.
Abnormalities in neurotransmitter systems also play a role. Psychopaths show altered serotonin and dopamine functioning. This affects mood regulation and reward processing.
Genetic factors contribute to psychopathy risk. Twin studies indicate psychopathic traits are moderately to highly heritable. Specific gene variants linked to neurotransmitter function may increase susceptibility.
Brain Areas Associated With Psychopathy
The amygdala shows reduced activity in psychopaths. This region processes emotions, especially fear. Its dysfunction likely contributes to their lack of empathy and fear response.
The prefrontal cortex, crucial for decision-making and impulse control, functions abnormally. This may explain impulsive and antisocial behaviors.
The ventral striatum, involved in reward processing, shows heightened activity. This could drive the pursuit of immediate gratification.
General Brain Function and Structure
Functional MRI studies reveal altered connectivity between brain regions in psychopaths. The limbic system and prefrontal cortex show reduced communication.
White matter tracts connecting different brain areas display abnormalities. This impacts information flow between regions.
Overall brain structure differs in psychopaths. They tend to have less gray matter volume in multiple areas. This affects neural processing and cognitive functions.
Neuroimaging techniques like fMRI and PET scans help visualize these differences. They provide insights into the unique neural patterns associated with psychopathy.
Psychopathy and the Prefrontal Cortex
The prefrontal cortex plays a crucial role in psychopathy, with specific regions showing altered structure and function. These differences contribute to the behavioral and emotional traits characteristic of psychopathic individuals.
Role of the Ventromedial Prefrontal Cortex
The ventromedial prefrontal cortex (vmPFC) is integral to emotional processing and decision-making. In psychopaths, this region shows reduced connectivity with the amygdala, impacting empathy and guilt.
This disconnection may explain the lack of remorse and callousness often observed in psychopathic behavior. Brain imaging studies have revealed decreased gray matter volume in the vmPFC of individuals with psychopathic traits.
The vmPFC's impaired function also affects moral reasoning and social behavior. Psychopaths often struggle with value-based decision-making and show diminished responses to others' distress.
Dorsolateral Prefrontal Cortex Involvement
The dorsolateral prefrontal cortex (dlPFC) is associated with executive functions, including planning and impulse control. In psychopaths, this region often exhibits abnormal activity patterns.
Functional MRI studies have shown reduced activation in the dlPFC during tasks requiring self-control or consideration of long-term consequences. This may contribute to the impulsivity and poor behavioral regulation seen in psychopathy.
The dlPFC also plays a role in attention and working memory. Some research suggests psychopaths may have enhanced cognitive abilities in certain areas, possibly linked to dlPFC function.
Orbitofrontal Cortex Connectivity
The orbitofrontal cortex (OFC) is crucial for reward processing and decision-making. In psychopathy, this region shows altered connectivity patterns with other brain areas.
Reduced connectivity between the OFC and amygdala may impair the ability to learn from punishment or negative outcomes. This can lead to persistent antisocial behavior despite negative consequences.
The OFC is also involved in impulse control and social behavior. Abnormalities in this region may contribute to the manipulative and socially inappropriate actions often seen in psychopaths.
Emotional Processing and Regulation in Psychopaths
Psychopaths exhibit distinct patterns in emotional processing and regulation. These differences manifest in amygdala function, empathy, moral judgment, and emotion regulation abilities.
Amygdala Function and Psychopathy
The amygdala plays a crucial role in emotional processing and fear responses. In psychopaths, this brain region shows reduced activity during emotional tasks.
Neuroimaging studies have revealed decreased activation in the right amygdala of psychopathic individuals when viewing emotional stimuli. This diminished response may contribute to their reduced fear sensitivity and emotional blunting.
Psychopaths often display a lack of physiological arousal to threatening or distressing stimuli. This blunted amygdala response could explain their fearlessness and tendency to engage in risky behaviors.
Empathy and Moral Judgment
Psychopaths typically struggle with empathy and moral decision-making. These deficits are linked to abnormal neural activity in key brain regions.
Studies show reduced activation in areas associated with empathy, such as the anterior insula and anterior cingulate cortex, when psychopaths observe others in distress. This may explain their callousness and lack of concern for others' feelings.
Moral judgment tasks reveal atypical patterns of brain activation in psychopaths. They often rely more on cognitive processes rather than emotional responses when making moral decisions.
The reduced emotional input during moral reasoning may contribute to their disregard for social norms and lack of conscience.
Emotion Regulation Deficits
Psychopaths often struggle with regulating their emotions effectively. This difficulty stems from abnormalities in brain regions responsible for emotional control.
Neuroimaging research has found altered connectivity between the prefrontal cortex and limbic regions in psychopaths. This disrupted communication may impair their ability to modulate emotional responses appropriately.
Psychopaths frequently exhibit impulsive and aggressive behaviors. These actions may result from poor emotion regulation skills and difficulty inhibiting negative emotions.
Treatment approaches for psychopathy often focus on improving emotion regulation abilities through cognitive-behavioral techniques and skills training.
Decision-Making and Impulse Control
Psychopaths exhibit distinct patterns in decision-making and impulse control due to differences in brain structure and function. These differences affect their ability to process rewards, regulate behavior, and consider long-term consequences.
Anterior Insula and Decision-Making
The anterior insula plays a crucial role in decision-making processes. In psychopaths, this region shows reduced activation during decision tasks. This may contribute to their impaired ability to evaluate risks and rewards effectively.
Neuroimaging studies have revealed decreased grey matter volume in the anterior insula of psychopathic individuals. This structural difference correlates with deficits in emotional processing and decision-making.
Psychopaths often make choices based on immediate gratification rather than considering long-term outcomes. This short-sighted decision-making style is linked to dysfunction in the anterior insula and related brain networks.
Self-Control and Delayed Gratification
Psychopaths typically struggle with self-control and delayed gratification. The prefrontal cortex, particularly the orbitofrontal region, is critical for these abilities.
Research has shown reduced grey matter in the orbitofrontal cortex of psychopathic individuals. This structural difference may explain their difficulty in restraining impulses and waiting for future rewards.
The dopamine system, which regulates reward processing, also functions abnormally in psychopaths. This dysregulation can lead to:
Increased reward-seeking behavior
Reduced sensitivity to punishment
Difficulty learning from negative consequences
These factors combine to create a pattern of poor self-control and an inability to delay gratification in psychopathic individuals.
Impulsivity and Aggression
Impulsivity and aggression are hallmark traits of psychopathy. These behaviors are linked to dysfunction in multiple brain regions, including the amygdala and prefrontal cortex.
Psychopaths show reduced activation in the amygdala when processing emotional stimuli. This blunted response may contribute to their lack of fear and increased risk-taking behavior.
The prefrontal cortex, responsible for impulse control, exhibits abnormal activity in psychopaths. This dysfunction can lead to:
Difficulty inhibiting inappropriate responses
Increased aggressive outbursts
Poor behavioral regulation
Neurochemical imbalances, particularly in serotonin levels, have also been implicated in the impulsive and aggressive tendencies of psychopaths.
Antisocial Behavior and Violence
Psychopathy is closely linked to antisocial behavior and violence. Research has uncovered connections between psychopathic traits, criminal acts, and aggressive tendencies.
Relationship Between Psychopathy and Violence
Psychopaths exhibit a higher likelihood of engaging in violent behavior. Studies show they often lack empathy and remorse, making them more prone to aggression. Their impulsivity and need for stimulation can lead to reckless, violent acts.
Brain imaging reveals reduced activity in areas associated with emotional processing and impulse control. This may contribute to their violent tendencies. Psychopaths also demonstrate diminished fear responses, potentially explaining their boldness in committing violent crimes.
Some research indicates psychopaths are responsible for a disproportionate amount of violent crime. Their charm and manipulation skills can make their violence more calculated and premeditated.
Antisocial Personality Disorder
Antisocial Personality Disorder (ASPD) shares traits with psychopathy but is a distinct diagnosis. Individuals with ASPD often display:
Disregard for social norms and laws
Impulsivity and aggression
Lack of remorse
Irresponsibility
Deceitfulness
ASPD is more prevalent than psychopathy, affecting 2-4% of the general population. While not all people with ASPD are psychopaths, most psychopaths meet the criteria for ASPD.
Brain scans of individuals with ASPD show structural and functional abnormalities in areas governing emotion, impulse control, and decision-making.
Criminal Psychopathy and Convictions
Psychopaths make up a significant portion of the prison population, estimated at 15-25%. They are more likely to commit violent crimes and reoffend after release. Criminal psychopaths often:
Start offending at a younger age
Have more diverse criminal records
Commit more instrumental (planned) violence
Studies indicate psychopaths are 2.5 times more likely to be released from jail despite high recidivism rates. This is partly due to their ability to manipulate parole boards.
Neuroimaging research on incarcerated psychopaths shows reduced gray matter in brain regions linked to empathy and moral reasoning. These biological factors may contribute to their criminal behavior and difficulty with rehabilitation.
Psychopathy in the Brain: Neuroimaging Studies
Neuroimaging techniques have provided valuable insights into the brain structures and functions associated with psychopathy. These studies reveal distinct patterns of brain activity and structural differences in individuals with psychopathic traits.
Magnetic Resonance Imaging Findings
Magnetic resonance imaging (MRI) has uncovered key brain abnormalities in psychopaths. Structural MRI studies show reduced gray matter volume in the amygdala, a region crucial for emotional processing and fear conditioning. The prefrontal cortex, responsible for decision-making and impulse control, also exhibits decreased volume.
Functional MRI research reveals altered activity patterns during tasks involving emotion, morality, and empathy. Psychopaths show reduced activation in the amygdala when viewing emotional faces or distressing images. The ventromedial prefrontal cortex, important for moral reasoning, displays diminished activity during moral decision-making tasks.
These findings suggest impaired emotional processing and moral judgment in psychopathy.
Default Mode Network and Psychopathy
The default mode network (DMN) plays a role in self-reflection, empathy, and social cognition. Neuroimaging studies indicate abnormalities in DMN connectivity among psychopaths.
Functional connectivity between key DMN regions, such as the medial prefrontal cortex and posterior cingulate cortex, is reduced in individuals with psychopathic traits. This decreased connectivity correlates with impaired empathy and self-referential processing.
Task-based fMRI studies show atypical DMN deactivation during cognitive tasks, suggesting difficulties in switching between internally and externally focused attention. These alterations may contribute to the lack of empathy and self-centered behavior characteristic of psychopathy.
Structural and Functional Brain Differences
Neuroimaging reveals both structural and functional brain differences in psychopathy. Structurally, reduced gray matter volume is observed in:
Amygdala
Hippocampus
Prefrontal cortex
Temporal lobe
White matter integrity is also compromised, particularly in tracts connecting the prefrontal cortex and limbic regions.
Functionally, psychopaths exhibit:
Decreased amygdala reactivity to emotional stimuli
Reduced activation in empathy-related brain regions
Altered connectivity between prefrontal and limbic areas
These differences likely contribute to the emotional deficits, impulsivity, and antisocial behavior seen in psychopathy. Understanding these neurobiological correlates may inform future interventions and risk assessment strategies.
Integrating Genetics and Environment
Psychopathy arises from a complex interplay of genetic predispositions and environmental influences. Recent research illuminates how these factors shape brain structure and function in individuals with psychopathic traits.
The Genetics of Psychopathy
Genetic studies reveal a heritable component to psychopathy. Twin and family studies estimate that genetic factors account for 40-60% of the variance in psychopathic traits.
Specific gene variants associated with psychopathy include those involved in neurotransmitter systems like serotonin and dopamine. The MAOA gene, which regulates monoamine oxidase levels, has been linked to aggression and antisocial behavior.
Neuroimaging research shows that certain genetic variations correlate with structural and functional brain differences in psychopathic individuals. For example, some gene variants are associated with reduced gray matter volume in the amygdala and other limbic regions.
Psychopathy and Environmental Factors
Environmental influences play a crucial role in shaping psychopathic traits. Early childhood experiences, particularly abuse, neglect, and trauma, can significantly impact brain development and behavior.
Harsh or inconsistent parenting practices are linked to increased callous-unemotional traits in children. Exposure to violence and criminal behavior in the family or community also contributes to the development of psychopathic tendencies.
Neurobiological studies show that adverse childhood experiences can alter brain structure and function. This includes changes in stress response systems, emotion regulation circuits, and reward processing pathways.
Interaction Between Genetics and Environment
Genetic and environmental factors do not operate in isolation but interact in complex ways to influence psychopathy. Gene-environment interactions occur when genetic predispositions modulate the impact of environmental experiences.
For instance, individuals with certain genetic variants may be more susceptible to developing psychopathic traits in response to childhood maltreatment. Conversely, protective environmental factors can mitigate genetic risks.
Epigenetic mechanisms provide a biological basis for these interactions. Environmental experiences can lead to changes in gene expression without altering the underlying DNA sequence. This helps explain how early life experiences can have long-lasting effects on brain function and behavior.
Clinical Applications and Interventions
Identifying and managing psychopathy involves specialized assessment tools, therapeutic approaches, and ongoing research into potential biomarkers. These clinical applications aim to improve diagnosis, treatment, and understanding of psychopathic traits.
Assessing Psychopathy
The Hare Psychopathy Checklist-Revised (PCL-R) is the gold standard for assessing psychopathy. This 20-item clinical rating scale evaluates interpersonal, affective, and behavioral features. Trained professionals conduct semi-structured interviews and review collateral information to score each item.
Other assessment tools include:
Psychopathy Personality Inventory (PPI)
Triarchic Psychopathy Measure (TriPM)
Self-Report Psychopathy Scale (SRP)
These instruments help clinicians identify psychopathic traits in various settings, including forensic and clinical contexts. Accurate assessment is crucial for treatment planning and risk management.
Therapeutic Approaches and Treatments
Treating psychopathy presents significant challenges due to the disorder's ingrained nature. Traditional psychotherapy often shows limited effectiveness. However, some approaches have shown promise:
Cognitive-behavioral therapy (CBT): Focuses on changing harmful thought patterns and behaviors
Mentalization-based treatment: Aims to improve empathy and emotional awareness
Reward-oriented interventions: Target the reward-seeking aspects of psychopathy
Early intervention programs for at-risk youth may help prevent the development of severe psychopathic traits. These programs often focus on:
Emotional regulation skills
Empathy training
Impulse control techniques
Medication is not a primary treatment for psychopathy but may be used to manage specific symptoms or co-occurring disorders.
Potential Biomarkers and Future Research
Identifying reliable biomarkers for psychopathy could revolutionize diagnosis and treatment. Current research focuses on:
Neuroimaging: fMRI studies reveal abnormalities in brain regions associated with emotion processing and decision-making
Genetic markers: Exploring genetic variations linked to psychopathic traits
Physiological indicators: Examining autonomic nervous system responses to emotional stimuli
Future research aims to:
Develop more targeted interventions based on neurobiological findings
Explore the potential for neurofeedback and brain stimulation techniques
Investigate epigenetic factors influencing the expression of psychopathic traits
Advances in these areas may lead to more personalized and effective treatments for individuals with psychopathic traits.