Prevalence and Distribution of Hoarding Disorder Worldwide
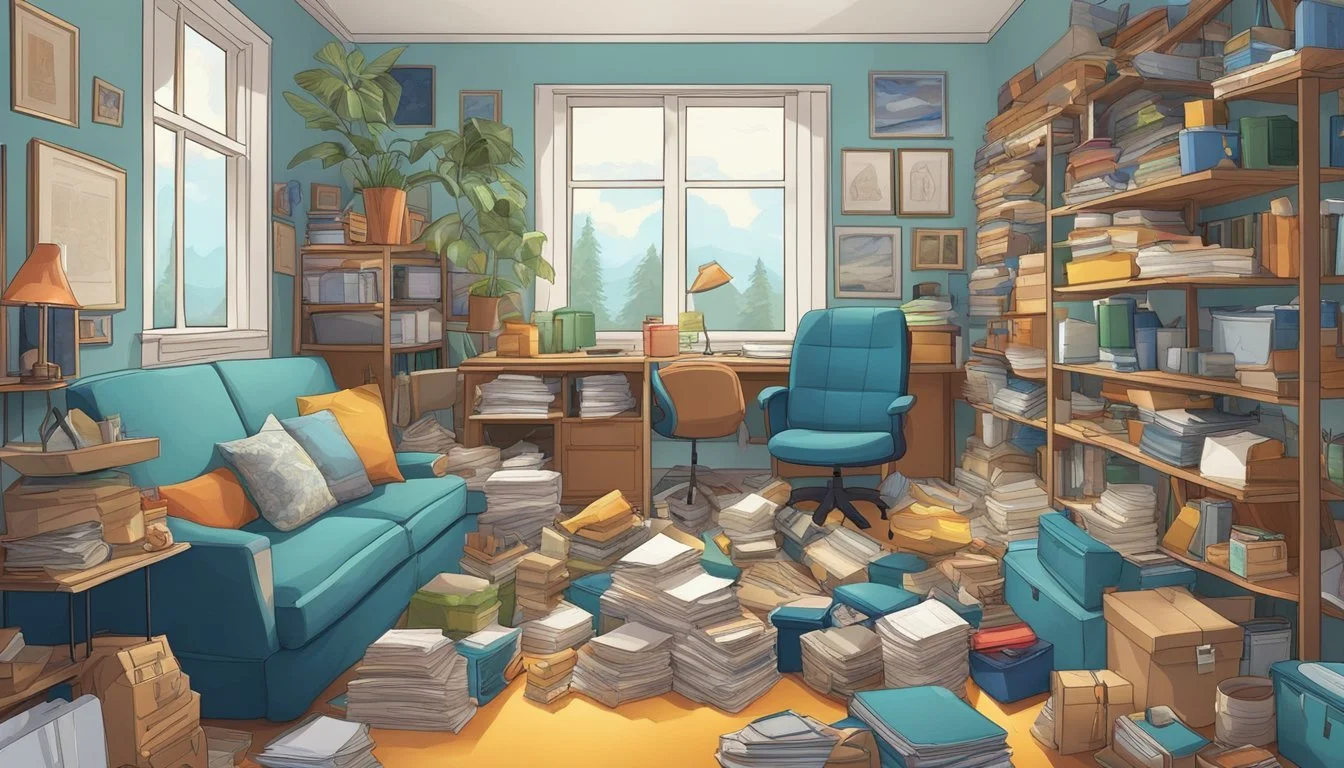
Hoarding disorder, a complex mental health condition, affects millions of people worldwide. This persistent difficulty discarding possessions, regardless of their actual value, can lead to significant impairment in daily functioning and quality of life.
Recent epidemiological studies estimate the prevalence of hoarding disorder to be between 2% and 6% of the general population. The wide range reflects the challenges in accurately assessing and diagnosing this condition. Interestingly, some research suggests that hoarding behaviors may be more common in men than women, though further investigation is needed to confirm this trend.
Recognized as a distinct disorder in the DSM-5, hoarding disorder is now understood to be separate from obsessive-compulsive disorder (OCD) in the majority of cases. This distinction has important implications for treatment approaches and outcomes. As research in this field continues to evolve, a clearer picture of hoarding disorder's epidemiology and its impact on various populations is emerging.
Understanding Hoarding Disorder
Hoarding disorder is a complex mental health condition characterized by persistent difficulty discarding possessions, regardless of their actual value. This results in the accumulation of items that congest living areas and cause significant distress or impairment in daily functioning.
Definition and DSM-5 Criteria
Hoarding disorder was officially recognized as a distinct diagnosis in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The American Psychiatric Association established specific criteria for diagnosis:
Persistent difficulty discarding possessions
Perceived need to save items and distress associated with discarding them
Accumulation of possessions that congest living areas
Clinically significant distress or impairment in functioning
These criteria help differentiate hoarding disorder from normal collecting behaviors or situational clutter.
Symptomatology and Diagnosis
Individuals with hoarding disorder experience intense anxiety when attempting to discard items. They often have difficulty organizing possessions and making decisions about what to keep or discard.
Common symptoms include:
Excessive acquisition of new items
Inability to use living spaces for their intended purposes
Social isolation due to embarrassment about living conditions
Impaired decision-making regarding possessions
Diagnosis typically involves a comprehensive psychiatric evaluation, including assessment of the living environment and impact on daily functioning.
Hoarding vs. Collecting
While hoarding and collecting may seem similar, they are distinct behaviors:
Hoarding Collecting Disorganized accumulation Organized acquisition Causes distress and impairment Brings joy and satisfaction Difficulty discarding items Willingness to sell or trade items Cluttered, unusable living spaces Displayed or stored collections
Collectors typically take pride in their collections and maintain organization. Hoarders often feel overwhelmed by their possessions and struggle to manage them effectively.
Epidemiological Insights
Hoarding disorder affects a significant portion of the population, with varying prevalence rates across different demographics. Research has shed light on its occurrence, population distribution, and common co-existing conditions.
Prevalence Estimates
Recent epidemiological studies provide a clearer picture of hoarding disorder's prevalence. Meta-analyses and systematic reviews estimate the disorder affects between 2% and 6% of the general population. This range reflects variations in diagnostic criteria and assessment methods across studies.
A systematic review of community samples found a weighted prevalence of 2.5%. However, rates tend to be higher in older adults, with some studies reporting prevalence up to 6% in individuals over 55 years old.
Prevalence estimates may be influenced by factors such as:
Diagnostic thresholds
Self-reporting biases
Cultural differences in defining clutter
Demographic Variations
Hoarding disorder manifests across diverse demographic groups, though certain patterns emerge. Age appears to be a significant factor, with symptom severity often increasing over time.
Key demographic findings include:
Onset typically occurs in childhood or adolescence
Symptoms usually become clinically significant by mid-adulthood
Higher prevalence rates in older adults
Gender differences are less pronounced, with most studies finding similar rates between males and females. Socioeconomic status and education level do not seem to be strong predictors of hoarding behavior.
Research on ethnic and cultural variations remains limited. Some studies suggest comparable prevalence rates across different ethnic groups, but more research is needed to understand potential cultural influences on hoarding behaviors and their recognition.
Comorbidity Factors
Hoarding disorder frequently co-occurs with other mental health conditions. Understanding these comorbidities is crucial for effective diagnosis and treatment.
Common comorbid conditions include:
Depression (up to 50% of cases)
Anxiety disorders (24-42%)
Obsessive-compulsive disorder (OCD) (20-30%)
Attention deficit hyperactivity disorder (ADHD) (28%)
While historically associated with OCD, recent research shows hoarding disorder is distinct, occurring independently in 60-80% of cases. This distinction is reflected in separate diagnostic criteria in the DSM-5.
Comorbidities can complicate treatment approaches and outcomes. Individuals with hoarding disorder and comorbid conditions often experience more severe symptoms and greater functional impairment, highlighting the need for comprehensive assessment and tailored interventions.
Risk Factors and Onset
Hoarding disorder typically emerges in childhood or adolescence and progresses gradually over time. Several key factors contribute to its development and persistence, including genetic predisposition, early life experiences, and cognitive-emotional patterns.
Genetics and Heritability
Hoarding disorder tends to run in families. Studies suggest a heritability rate of 50-60% for hoarding symptoms. This indicates a significant genetic component in the disorder's etiology.
Individuals with first-degree relatives who hoard are more likely to develop the condition themselves. Twin studies have further supported the role of genetics in hoarding behavior.
Research has identified specific genes potentially linked to hoarding tendencies, though more investigation is needed to fully understand these genetic factors.
Early Life Experiences
Traumatic events and disrupted attachment in childhood can increase the risk of developing hoarding disorder. Experiences such as loss, abuse, or neglect may contribute to the onset of hoarding behaviors.
Some individuals with hoarding disorder report difficult family relationships or unstable living situations during their formative years. These experiences may lead to using possessions as a source of comfort or security.
The average age of onset for hoarding symptoms is between 11 and 15 years old. However, the full disorder often doesn't manifest until later in adulthood.
Cognitive and Emotional Aspects
Certain cognitive patterns and emotional difficulties are associated with hoarding disorder. These include:
Attention deficits
Impaired decision-making skills
Difficulties with categorization and organization
Problems with emotional regulation
Individuals with hoarding disorder often experience intense emotional attachments to objects. They may also struggle with anxiety, depression, or perfectionism.
Executive function deficits, particularly in areas of planning and task completion, are common in those with hoarding tendencies. These cognitive challenges can make it difficult to organize and discard items.
Memory issues may play a role, with some individuals keeping objects as reminders or due to fears of forgetting important information.
Clinical Assessment and Measurement
Accurate diagnosis and assessment of hoarding disorder require specialized tools and approaches. Clinicians utilize a combination of structured interviews, self-report measures, and home visits to evaluate symptom severity and functional impairment.
Diagnosis and Screening Tools
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides criteria for diagnosing hoarding disorder. Clinicians often use structured diagnostic interviews like the Structured Clinical Interview for DSM-5 (SCID-5) to assess these criteria systematically.
Screening tools can help identify potential cases. The Hoarding Rating Scale-Interview (HRS-I) is a brief, clinician-administered measure that assesses key features of hoarding.
For a more comprehensive evaluation, the Structured Interview for Hoarding Disorder (SIHD) covers all DSM-5 criteria and associated features.
Self-Report and Interview Approaches
Self-report questionnaires play a crucial role in assessing hoarding symptoms. The Saving Inventory-Revised (SI-R) is widely used to measure difficulty discarding, excessive acquisition, and clutter.
The Clutter Image Rating (CIR) uses a series of photographs to assess clutter severity in different rooms of the home.
Clinical interviews provide in-depth information about hoarding behaviors and their impact. The Yale-Brown Obsessive Compulsive Scale modified for hoarding (Y-BOCS-H) assesses time spent, interference, distress, and control over hoarding symptoms.
Assessment Challenges
Evaluating hoarding disorder presents unique challenges. Individuals with hoarding often lack insight into the severity of their condition, potentially underreporting symptoms.
Home visits are essential for accurately assessing clutter and safety hazards. However, some individuals may be reluctant to allow professionals into their homes.
Differentiating hoarding from normal collecting or other mental health conditions can be complex. A multi-method assessment approach, including clinical interviews, self-report measures, and home visits, improves diagnostic accuracy.
Cultural factors can influence the interpretation of hoarding behaviors, necessitating culturally sensitive assessment approaches.
Impact and Implications of Hoarding Disorder
Hoarding disorder has far-reaching consequences that extend beyond cluttered living spaces. It affects individuals' health, relationships, and economic stability while posing challenges for treatment and intervention.
Functional and Health Outcomes
Hoarding disorder significantly impairs daily functioning and quality of life. Individuals struggle to use living spaces for their intended purposes, leading to difficulties in basic activities like cooking, sleeping, and personal hygiene. The accumulation of items increases the risk of falls, fires, and unsanitary conditions.
Physical health problems are common among those with hoarding disorder. Respiratory issues may arise from dust and mold. Poor nutrition can result from limited access to kitchen facilities. Chronic pain conditions often develop due to navigating cluttered environments.
Mental health is also affected. Depression, anxiety, and social isolation frequently co-occur with hoarding. In some cases, hoarding behaviors may be an early sign of dementia or other cognitive decline.
Social and Economic Consequences
Hoarding disorder strains relationships with family, friends, and neighbors. Conflicts arise over clutter, safety concerns, and embarrassment about home conditions. Social withdrawal is common as individuals avoid inviting others to their homes.
Financial impacts can be severe. Excessive acquiring leads to debt, while neglected home maintenance reduces property values. Eviction and homelessness are real risks for some. Employment may be affected if hoarding behaviors extend to the workplace.
Communities face increased costs for interventions, clean-ups, and social services. Local governments may need to address code violations, pest control issues, and public health concerns stemming from severe hoarding cases.
Treatment Considerations
Treating hoarding disorder presents unique challenges. Many individuals lack insight into the severity of their condition, resisting intervention attempts. Strong emotional attachments to possessions complicate the discarding process.
Cognitive-behavioral therapy (CBT) is the primary evidence-based treatment. It focuses on changing thoughts and behaviors related to acquiring, saving, and discarding items. Skills training in organization and decision-making is often incorporated.
Medication may play a supportive role. Some studies suggest venlafaxine and other antidepressants can reduce hoarding symptoms. However, pharmacotherapy alone is generally insufficient.
Treatment outcomes vary. Improvement often occurs gradually, with full remission being rare. Ongoing support and booster sessions are typically needed to maintain gains and prevent relapse.
Community and Public Health Approaches
Hoarding disorder poses significant challenges for communities and public health systems. Addressing this complex issue requires multi-faceted strategies tailored to diverse populations.
Prevalence in Diverse Communities
Hoarding disorder affects people across various demographic groups. The SELCOH study in London found prevalence rates of 1.5% in an ethnically diverse community sample. This research highlights the need to consider cultural factors when assessing hoarding behaviors.
Urban areas may see higher rates due to population density and housing constraints. Rural communities face unique challenges in identifying and supporting individuals with hoarding disorder due to geographic isolation.
Socioeconomic status can impact hoarding prevalence. Lower-income neighborhoods may have fewer resources to address the problem, while affluent areas might have better-hidden cases.
Public Health Strategies
Public health approaches to hoarding disorder focus on prevention, early intervention, and harm reduction. Task forces combining mental health professionals, social services, and first responders have proven effective in many cities.
Key strategies include:
Home safety assessments
Decluttering assistance programs
Support groups for individuals and families
Collaborative care models involving primary care physicians
Zoning laws and housing codes play a crucial role in addressing severe cases. Some municipalities have implemented specialized hoarding units to coordinate responses and ensure compliance with health and safety regulations.
Awareness and Education Efforts
Raising public awareness is essential for early identification and intervention. Educational programs target various groups:
Healthcare providers
Social workers
Teachers
Housing authorities
General public
These initiatives aim to reduce stigma, explain the complexities of hoarding disorder, and provide resources for help. Public service announcements, community workshops, and online resources help disseminate accurate information.
Training for professionals focuses on assessment tools, intervention techniques, and ethical considerations. Continuing education programs ensure that practitioners stay updated on best practices for treating hoarding disorder.