Classification of Compulsive Accumulation Behaviors
Hoarding disorder is a complex mental health condition that affects approximately 6% of the population. Individuals with this disorder experience an overwhelming urge to acquire and keep items, regardless of their actual value. This compulsive behavior can lead to significant clutter, impaired living conditions, and distress when attempting to discard possessions.
The disorder falls under the category of anxiety-related conditions in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). People with hoarding disorder often struggle with decision-making, organization, and attachment to objects. These challenges can result in unsafe living environments, strained relationships, and social isolation.
Recognizing the signs of hoarding disorder is crucial for early intervention and treatment. Mental health professionals can diagnose the condition through careful assessment of symptoms and their impact on daily functioning. Effective treatments, such as cognitive-behavioral therapy, can help individuals manage their hoarding tendencies and improve their quality of life.
Understanding Hoarding Disorder
Hoarding disorder is a complex mental health condition characterized by persistent difficulty discarding possessions and excessive acquisition behaviors. It can significantly impact a person's quality of life and living spaces.
Definition and Criteria
Hoarding disorder is recognized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a distinct condition. It involves persistent difficulty parting with possessions, regardless of their actual value. This difficulty stems from a perceived need to save items and distress associated with discarding them.
The criteria for diagnosis include:
Persistent difficulty discarding possessions
Strong urges to save items and distress when attempting to discard them
Accumulation of items that congest living areas
Significant distress or impairment in daily functioning
These symptoms must not be better explained by another mental disorder or medical condition.
Signs and Symptoms
Key signs of hoarding disorder include:
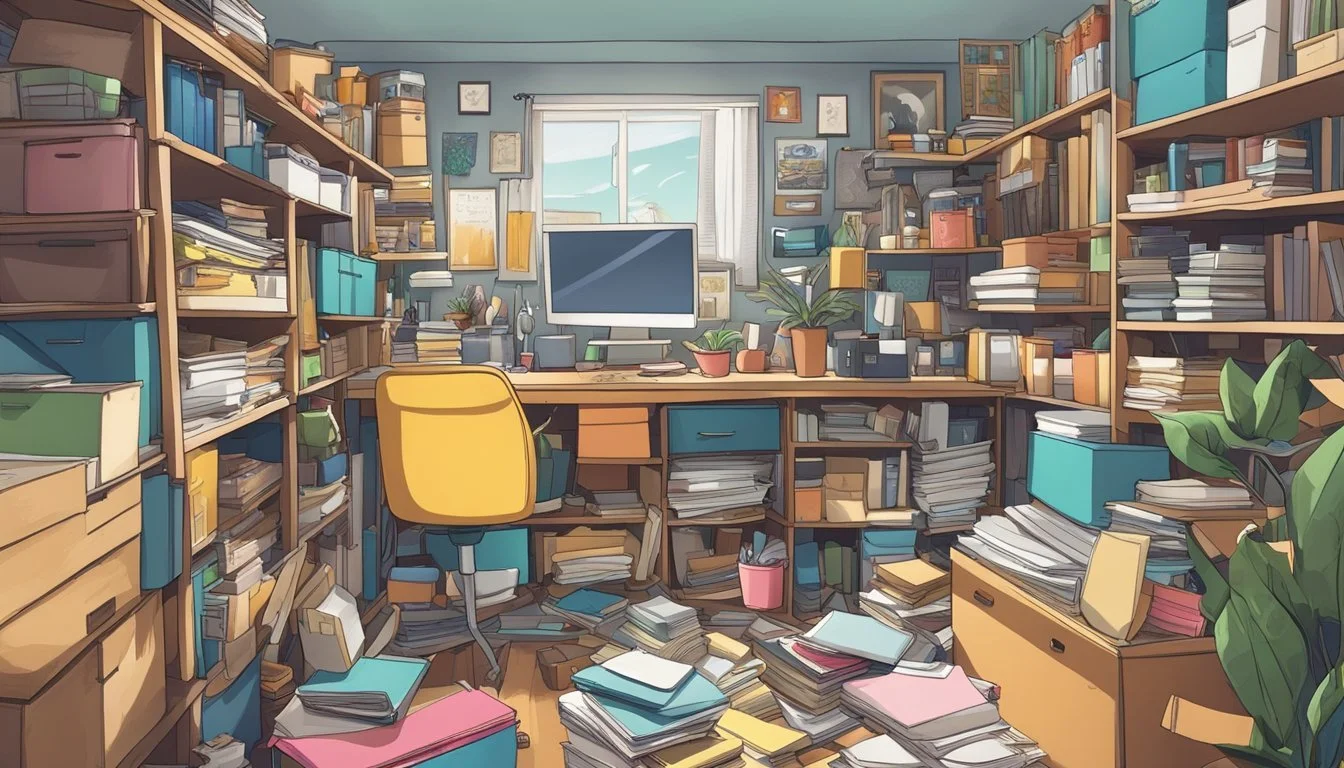
Cluttered living spaces that prevent normal use of rooms
Difficulty organizing items
Indecisiveness about what to keep or discard
Excessive acquisition of unnecessary items
Emotional symptoms often involve:
Anxiety when attempting to discard items
Feeling overwhelmed by possessions
Shame or embarrassment about living conditions
Behavioral symptoms may include:
Compulsive buying
Collecting free items excessively
Difficulty categorizing or organizing possessions
Common Misconceptions
Hoarding is often misunderstood. Common misconceptions include:
Hoarding is just being messy or disorganized
People who hoard are lazy
Hoarding only affects older adults
In reality, hoarding is a complex disorder that can affect people of all ages. It's not a choice or a sign of laziness, but a mental health condition requiring professional help.
Another misconception is that forcibly removing possessions solves the problem. This approach can cause significant distress and doesn't address the underlying issues.
Hoarding is also different from collecting. Collectors typically organize their items and display them proudly, while those with hoarding disorder often experience shame and their items create disarray.
Prevalence and Demographics
Hoarding disorder affects a significant portion of the population, with estimates ranging from 2-6% in the United States. The condition impacts individuals across various age groups, socioeconomic backgrounds, and geographic locations.
Age of Onset
Hoarding behaviors typically emerge during adolescence, often around ages 11-15. The symptoms tend to worsen over time, with many individuals not seeking treatment until middle age or later. By age 50, hoarding patterns are often well-established.
Studies show that hoarding severity increases with age. Older adults may face greater challenges due to accumulated possessions and declining physical abilities to manage clutter.
Socioeconomic Factors
Hoarding disorder affects people across all income levels and educational backgrounds. However, certain factors may influence its impact:
Employment: Hoarders may struggle to maintain steady jobs due to organizational difficulties.
Living arrangements: Many individuals with hoarding disorder live alone, which can exacerbate the problem.
Gender: Research suggests hoarding affects men and women equally, contrary to earlier beliefs of female predominance.
Financial strain often accompanies hoarding, as excessive acquisitions and inability to discard items can lead to debt and housing issues.
Geographic Variations
While hoarding occurs worldwide, most research has focused on Western countries. Urban areas may see higher reported rates due to:
Greater population density
Smaller living spaces highlighting clutter issues
Increased access to mental health services
Rural communities face unique challenges:
Less visibility of hoarding behaviors
Fewer resources for treatment and support
Larger properties allowing for more accumulation
Cultural factors can influence hoarding manifestations and help-seeking behaviors across different regions.
Causes and Risk Factors
The origins of hoarding disorder involve a complex interplay of genetic, environmental, and psychological factors. These elements contribute to the development and progression of hoarding behaviors.
Genetic Influences
Research suggests a genetic component to hoarding disorder. Studies have found that individuals with a family history of hoarding are more likely to develop the condition themselves. Twin studies indicate a heritability rate of approximately 50%, pointing to a significant genetic contribution.
Specific genes linked to hoarding tendencies have not been definitively identified. However, researchers have observed correlations between hoarding behaviors and variations in genes associated with serotonin regulation and decision-making processes.
Environmental Triggers
Environmental factors often play a crucial role in the onset and exacerbation of hoarding symptoms. Traumatic experiences or significant life stressors can trigger or worsen hoarding behaviors.
Common environmental triggers include:
Loss of a loved one
Divorce or relationship breakdown
Serious illness or injury
Financial hardship
Major life transitions
Childhood experiences, such as material deprivation or unstable living situations, may also contribute to the development of hoarding tendencies later in life.
Psychological Components
Psychological factors underpin many aspects of hoarding disorder. Cognitive patterns and emotional processes contribute to the difficulty in discarding items and the excessive acquisition behaviors characteristic of hoarding.
Key psychological components include:
Difficulty making decisions
Perfectionism and fear of making mistakes
Strong emotional attachments to possessions
Anxiety about forgetting or losing important information
Beliefs about the intrinsic value or potential usefulness of items
These psychological factors often interact with genetic predispositions and environmental stressors, creating a complex web of influences that shape hoarding behaviors.
Impact on Daily Life
Hoarding disorder significantly affects multiple aspects of a person's daily functioning. The accumulation of excessive items creates physical, emotional, and social challenges for those struggling with this condition.
Quality of Life
Individuals with hoarding disorder often experience a decline in their overall quality of life. Cluttered living spaces make it difficult to perform basic tasks like cooking, cleaning, and personal hygiene.
Movement through the home becomes restricted, limiting access to essential areas. Sleep quality may suffer due to overcrowded bedrooms. Financial strain can occur from purchasing unnecessary items or paying for storage units.
Hoarding behaviors frequently lead to increased stress and anxiety. The overwhelming nature of the clutter can cause feelings of shame, embarrassment, and isolation.
Family and Social Relationships
Hoarding disorder strains relationships with family members, friends, and neighbors. Loved ones may feel frustrated or helpless when attempts to help are met with resistance.
Conflicts arise over the state of the home and the individual's reluctance to discard items. Social interactions become limited as the person avoids inviting others to their cluttered living space.
Children in hoarding households may face challenges with schoolwork, playtime, and social development. In severe cases, child protective services may intervene if the home environment is deemed unsafe.
Household Safety
Hoarding creates numerous safety hazards within the home. Piles of items increase the risk of falls, especially for elderly individuals. Blocked exits pose a serious danger in emergency situations.
Fire risks are significantly elevated due to flammable materials and obstructed pathways. Electrical hazards may arise from overloaded outlets or damaged wiring hidden beneath clutter.
Unsanitary conditions often develop, leading to pest infestations and potential health issues. Mold growth and poor air quality can exacerbate respiratory problems. In extreme cases, structural damage to the home may occur from the weight of accumulated items.
Assessment and Diagnosis
Accurate assessment and diagnosis of hoarding disorder require a comprehensive approach. Mental health professionals use multiple methods to evaluate symptoms, severity, and impact on daily functioning.
Clinical Interviews
Trained clinicians conduct structured interviews to gather essential information about hoarding behaviors. They explore the individual's history, current living conditions, and emotional attachments to possessions. Questions focus on acquisition patterns, difficulty discarding items, and clutter levels in the home. The interview also assesses functional impairment in daily activities and relationships.
Clinicians may use the Structured Interview for Hoarding Disorder (SIHD) to systematically evaluate symptoms based on DSM-5 criteria. This tool helps differentiate hoarding disorder from other conditions with similar presentations.
Psychological Assessment Tools
Standardized questionnaires and rating scales provide valuable data for diagnosis and treatment planning. The Saving Inventory-Revised (SI-R) is a 23-item self-report measure that assesses three key aspects of hoarding: difficulty discarding, excessive acquisition, and clutter.
The Clutter Image Rating (CIR) uses a series of photographs to visually represent clutter levels in different rooms. Patients select images that best match their living spaces, offering an objective measure of clutter severity.
Other useful tools include:
Hoarding Rating Scale (HRS)
Activities of Daily Living in Hoarding (ADL-H)
Saving Cognitions Inventory (SCI)
Differential Diagnosis
Mental health professionals must carefully distinguish hoarding disorder from other conditions with similar symptoms. Obsessive-compulsive disorder (OCD) can involve hoarding behaviors, but the underlying motivations and thought patterns differ.
Depression may lead to clutter accumulation due to lack of energy or motivation, rather than emotional attachment to items. Attention-deficit/hyperactivity disorder (ADHD) can result in disorganization that resembles hoarding.
Clinicians also consider medical conditions that might contribute to hoarding behaviors, such as dementia or brain injuries. A thorough evaluation helps ensure accurate diagnosis and appropriate treatment planning.
Treatment Approaches
Effective treatment for hoarding disorder involves a multifaceted approach. Psychotherapy, medication, and supportive interventions are key components in helping individuals manage their symptoms and improve their quality of life.
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy (CBT) is the primary treatment for hoarding disorder. It focuses on changing thought patterns and behaviors associated with excessive acquisition and difficulty discarding items. CBT helps individuals:
Identify and challenge unhelpful beliefs about possessions
Develop decision-making and organizational skills
Practice sorting and discarding items
Resist the urge to acquire new things
Therapists often conduct home visits to assess the living environment and provide hands-on assistance. CBT sessions may occur individually or in group settings, allowing participants to share experiences and support one another.
Medication Management
While no medications are specifically approved for hoarding disorder, certain drugs may help manage related symptoms. Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), can be beneficial for individuals experiencing:
Depression
Anxiety
Obsessive-compulsive tendencies
Medication is typically used in conjunction with psychotherapy for optimal results. A psychiatrist or healthcare provider can determine the most appropriate medication regimen based on individual needs and symptoms.
Supportive Interventions
Supportive interventions complement therapy and medication by addressing practical aspects of hoarding disorder. These may include:
Professional organizing services
Home health aides for cleaning and decluttering
Family therapy to improve relationships and communication
Support groups for individuals with hoarding disorder
Community resources, such as social workers and public health departments, can provide assistance with home safety and legal issues related to hoarding. Educational workshops on organizing, decision-making, and time management skills also prove helpful for many individuals.
Challenges in Treating Hoarding Disorder
Treating hoarding disorder presents unique obstacles that require specialized approaches. Therapists and healthcare providers face difficulties in engaging patients, addressing complex psychological factors, and managing associated health risks.
Resistance to Treatment
Individuals with hoarding disorder often struggle to recognize the severity of their condition. They may view their possessions as valuable or essential, making it challenging to accept help. This resistance can manifest as missed appointments or reluctance to allow home visits.
Cognitive distortions play a significant role in treatment resistance. Patients may overestimate the importance of items or fear negative consequences from discarding them. These beliefs can be deeply ingrained and difficult to challenge.
Anxiety and stress frequently accompany attempts to declutter or organize. The prospect of change can trigger intense emotional responses, leading to avoidance behaviors. Therapists must navigate these reactions carefully to maintain patient engagement.
Complications with Co-morbidity
Hoarding disorder rarely occurs in isolation. Common co-occurring conditions include depression, anxiety disorders, and OCD. These additional diagnoses can complicate treatment plans and recovery processes.
Mental health professionals must address multiple symptoms simultaneously. For example, treating depression may be necessary before tackling hoarding behaviors. This interplay requires a nuanced, multi-faceted approach to therapy.
Physical health issues often arise from cluttered living spaces. Respiratory problems, fall risks, and hygiene concerns may need immediate attention. Coordinating care with medical professionals becomes crucial in these cases.
Strategies for Engagement
Building trust is essential for effective treatment. Therapists must approach patients with empathy and understanding, acknowledging the emotional attachments to possessions. Non-judgmental communication helps create a safe environment for change.
Cognitive-behavioral therapy (CBT) techniques can be adapted for hoarding disorder. These may include exposure exercises, cognitive restructuring, and skills training. Gradual exposure to discarding items can help reduce anxiety over time.
Involving family members or support systems can enhance treatment outcomes. Education about hoarding disorder helps loved ones provide appropriate assistance. However, maintaining patient privacy and autonomy remains crucial throughout the process.
Strategies for Family Members
Family members play a crucial role in supporting individuals with hoarding disorder. Effective strategies involve understanding the condition and offering appropriate support.
Understanding the Disorder
Hoarding disorder is a complex mental health condition characterized by difficulty discarding possessions. It often stems from deep-seated emotional attachments or fears. Family members should educate themselves about the disorder's symptoms and causes.
Recognizing that hoarding is not laziness or stubbornness is essential. It's a genuine struggle for the affected person. Learning about the disorder helps family members approach the situation with empathy and patience.
Understanding triggers and thought patterns associated with hoarding can provide insights into the loved one's behavior. This knowledge forms the foundation for developing effective support strategies.
How to Offer Support
Supporting a family member with hoarding disorder requires a delicate balance of compassion and encouragement. Avoid forceful decluttering attempts, as these can cause distress and resistance.
Instead, focus on open, non-judgmental communication. Express concerns about safety and health risks calmly. Offer assistance in organizing belongings rather than insisting on discarding items.
Encourage professional help from therapists specializing in hoarding disorder. Family members can participate in therapy sessions to learn coping strategies and improve communication.
Set realistic goals and celebrate small victories. Help create a safer living environment by addressing immediate hazards. Patience is key, as progress may be slow but steady.
Organizational and Decluttering Techniques
Effective strategies for decluttering and organizing are essential for managing hoarding tendencies. These approaches help create order, maximize space, and establish sustainable habits.
Step-by-Step Guide to Decluttering
Start with small, manageable areas. Choose a single drawer or shelf to begin the decluttering process. Sort items into three categories: keep, donate, and discard.
Evaluate each item's usefulness and emotional value. Ask questions like "Have I used this in the past year?" or "Does this bring me joy?" to make informed decisions.
Set time limits for decluttering sessions. Work in 15-30 minute intervals to prevent overwhelm. Take breaks between sessions to recharge and refocus.
Create a staging area for sorted items. Use boxes or bags to separate keep, donate, and discard piles. Remove donate and discard items promptly to prevent second-guessing.
Organizational Systems
Implement a "one in, one out" rule. For every new item brought into the space, remove one existing item. This helps maintain balance and prevents accumulation.
Utilize vertical storage solutions. Install shelves, hanging organizers, or stackable bins to maximize space and keep floors clear.
Label storage containers clearly. Use category names or specific item descriptions to easily identify contents. This promotes accessibility and reduces the need to search through multiple containers.
Group similar items together. Create designated zones for different categories of possessions. This system makes it easier to locate items and prevents duplicate purchases.
Maintenance and Prevention Strategies
Schedule regular decluttering sessions. Set aside time weekly or monthly to review and organize possessions. Consistency prevents clutter from building up over time.
Implement a "maybe" box for items you're unsure about. Store these items for a set period, like 3-6 months. If unused during this time, consider donating or discarding them.
Create a donation station. Designate a specific area for items to be donated. When the space fills up, schedule a donation drop-off.
Practice mindful acquisition. Before purchasing new items, consider their necessity and long-term value. This helps reduce impulse buying and prevents unnecessary accumulation.
Legal and Ethical Considerations
Hoarding disorder intersects with various legal and ethical issues. Property laws, animal welfare concerns, and intervention ethics all come into play when addressing this complex condition.
Property Laws
Hoarding often violates local housing codes and zoning regulations. Excessive clutter can create fire hazards, structural damage, and unsanitary conditions. Municipalities may issue citations or condemn properties in severe cases.
Landlords face challenges evicting tenants with hoarding disorder due to disability protections. The Americans with Disabilities Act may require reasonable accommodations before eviction proceedings.
Property owners can be held liable for damages caused by hoarding, such as pest infestations affecting neighboring units. Insurance companies may deny coverage for hoarding-related claims, citing negligence.
Animal Hoarding Issues
Animal hoarding involves keeping numerous pets without proper care. It raises serious legal and ethical concerns regarding animal welfare.
Animal control agencies can seize neglected animals and press criminal charges for cruelty. Hoarders may face fines, jail time, and bans on future pet ownership.
Veterinary professionals have a duty to report suspected animal hoarding cases. Ethical dilemmas arise when client confidentiality conflicts with animal welfare obligations.
Rehabilitation efforts focus on education and monitoring rather than punishment. Some jurisdictions offer diversion programs to avoid criminal penalties if hoarders comply with treatment.
Ethics of Intervention
Forced cleanouts raise ethical questions about autonomy versus beneficence. Mental health professionals must balance respect for client choices with duty to prevent harm.
Involuntary treatment may be warranted if hoarding poses imminent danger. However, coercive interventions can damage therapeutic relationships and exacerbate symptoms.
Family members often struggle with ethical decisions about intervening. Setting boundaries while offering support is crucial. Seeking professional guidance can help navigate complex family dynamics.
Cognitive-behavioral therapy is the primary ethical treatment approach. It emphasizes collaborative goal-setting and gradual exposure to discarding items.
Resources and Support
Various resources and support options are available for individuals with hoarding disorder and their loved ones. These include support groups, educational materials, professional services, and specialized treatment programs.
Support Groups and Educational Materials
The International OCD Foundation (IOCDF) offers a comprehensive resource directory for hoarding disorder. This directory includes listings for support groups, therapists, and treatment programs. Support groups provide a safe space for individuals to share experiences and coping strategies. Many groups welcome both those with hoarding disorder and their family members.
Educational materials about hoarding disorder are available through mental health organizations and reputable online sources. These materials cover symptoms, causes, and treatment options. Some organizations offer webinars and workshops to help people better understand the condition and learn management techniques.
Professional Help and Services
Mental health professionals specializing in hoarding disorder play a crucial role in treatment. Cognitive behavioral therapy (CBT) is the primary treatment approach. Therapists trained in CBT help individuals challenge and change beliefs and behaviors related to hoarding.
Specialized hoarding cleanup services are available in many areas. These services often work in conjunction with mental health professionals to provide practical assistance. They help declutter and organize living spaces while respecting the individual's emotional needs.
Some clinics and hospitals offer specialized hoarding disorder treatment programs. These programs may combine therapy, medication management, and practical skills training. Treatment plans are typically tailored to each individual's specific needs and circumstances.